“This article originally appeared on www.stout.com.”

Ensure accurate coding and billing by reviewing the coding and compliance policies woven into a health system’s revenue cycle.
Because coding can be confusing and laborious it can often be overlooked and potentially not recognized as part of the revenue cycle process. Now more than ever before, coding reviews are an important component of a health system’s overall "value”-based payment continuum, due to continued scrutiny by Medicare/Medicaid and commercial payers. Health system executives are tasked with optimizing performance of and maximizing efficiency of the coding stage in the revenue cycle. Accurate coding leads to clean claims, which results in prompt reimbursement, and that’s why coding has a direct impact on the bottom line.
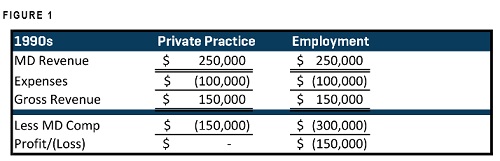
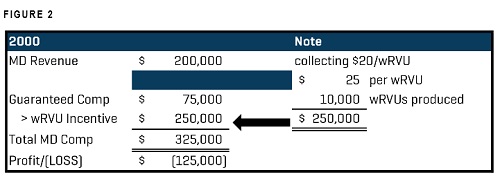
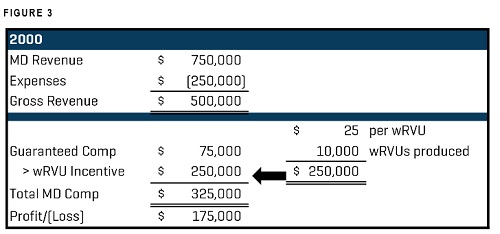
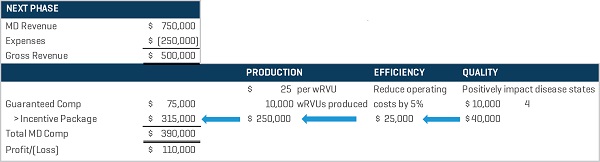
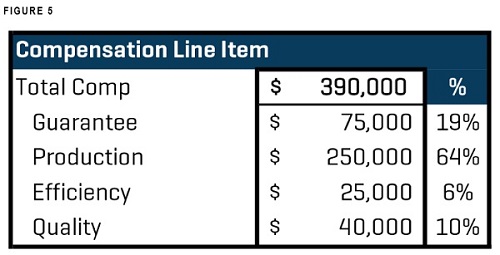
Coding is a moving target for many providers. Omnipresent and at times inconvenient and confusing, the ever-changing demands coupled with the risk of inaccuracy constantly challenges providers. With severity of care levels and clinical outcomes increasingly tied to “value,” reimbursements will inextricably link with accurate disease-state coding and documentation. Also, with provider compensation woven tightly to provider production (with emerging compensation models embracing quality and efficiency components, as well), accurate coding confirms both proper reimbursement to the system and accurate compensation for those providers on productivity models.
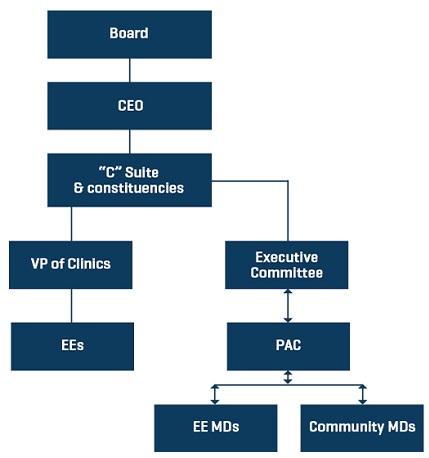
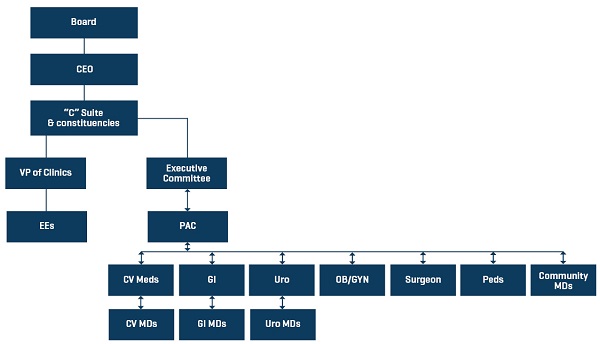
Educating providers mitigates downside risk to health systems and hospitals and offers leadership (the C-suite along with the physician executive team) the prophylactic of ongoing monitoring ensuring that the administrative/physician partnerships are cemented in a compliant manner.
Coding Compliance
A successful coding review and compliance plan should be crafted to define the hospital or health system’s investment and belief in coding compliance. A memorialization of the processes and procedures undertaken in a coding review enshrines that all constituents clearly understand the goals, objectives, and expectations of the hospital/system. Coding/compliance plans cannot be one-dimensional relying solely on documentation of services or an information technology solution. For instance, in a vacuum a provider can “pass” a coding assessment with proper documentation which generates work relative value units (wRVU). However, sometimes that productivity can be overly, and erroneously, robust given clinic hours, patient facing time, provider schedules, etc. Since most employed providers have a component of their compensation driven, at least in part, from a wRVU model, ensuring precise claim level of billing (e.g. a level 3 versus a level 5) offers physicians and health system leadership peace in the knowledge that claims, charges, and subsequent revenue are accurate.
Additionally, until block chain, “machine learning,” and other IT initiatives like artificial intelligence (AI) have firmly taken hold to “solve” coding and compliance issues, human-intervention will be required to certify that coding documentation aligns with patient facing time, required coding elements, and charting. EHRs can be dangerous when a user simply hap-hazardly “carries forward” a note which can offer a false sense of accuracy. Providers (physicians and APPs) must fully understand the rules and regulations of coding, especially in the critical nature of pay for value initiatives that are evolving over time. Additionally, and tangentially, carrying notes forward has potential med/mal exposure. All of that said, accurate coding is essential relative to severity of disease state, etc.
A Coding and Compliance Program - The "3 F's"
Frequency
Delineate a program of ongoing review and analysis. It should have well-defined expectations. The program should be structured with defined timelines, be diligent, and guarantee random sampling and a rotating sequence of providers (depending on group size) for review. In program development “acceptable” parameters should be constructed indicating varying rates of post-review monitoring and education. The program should be “owned” by a staff member (with backup) to ensure it is perpetual and robust.
Feedback
After reviews are performed, an expedient and concise feedback loop should be deployed displaying to providers deficiencies and providing education. For instance, if a provider “fails” 80% of his or her coding reviews for accuracy, he or she should be placed on a more frequent review process (every quarter?) as defined in the compliance plan to document a remediation process and catalogue improvement in accuracy.
The feedback loop should contain educational opportunities that celebrate successes and elucidate challenges. Providers should be counseled and offered “real time” assistance if coding issues or questions arise during the day.
Follow-up
The coding review should carry with it a robust follow-up plan ensuring that team members (from front desk to providers) understand that the plan is deployed and in force infusing into the culture a sense that the system or hospital takes, and will continue to take, coding compliance seriously. That is not to say that staff members should know that Dr. X failed his or her coding review. Instead, the message to staff should be that the system views coding compliance as a system-wide obligation and focus.
Stout’s coding/compliance leadership ties coding together with one point of contact to manage all aspects of review and education. Our seamless coding and compliance team delivers a variety of solutions based on client need. Stout associates manage outpatient, “pro fee” evaluation and management (E&M) and risk adjusted coding assessments and education, while deftly handling Ambulatory Payment Classification (APC), Diagnosis Resource Group (DRG), and Clinical Documentation Improvement (CDI) coding initiatives for inpatient coding. Additionally, we are adept at hospice and home care coding analyses. Our “borderless” approach empowers our team to rapidly address client needs by removing artificial “silos” that inhibit fluidity on multi-faceted projects running between health system, inpatient work and ambulatory reviews. Stout associates understand the congruency of in and outpatient facilities and can deliver reviews and offer a coding/compliance partner.
* To read more about Stout’s experience and how we provided a 15 to 1 return on a client’s initial investment by helping them improve on their revenuecycle, download our case study now.
Physician Compensation Value-Based Care Initiatives Bring Disruption
a href=http://www.wiederholdassoc.com/blog/2018/10/19/physician-executives-are-you-utilizing-their-talent>Physician Executives – Are You Utilizing Their Talent?
Connect with us on LinkedIn, join our Active Network Program and look at the other areas of connection we offer.