
Culture of Performance Excellence: A simplified Approach
Physician alignment, integration and engagement in integrated delivery systems are essential elements in navigating the complexity of healthcare service delivery. Healthcare organizations need a simplified approach to realize organizational vision of comprehensive and successful alignment and integration strategies. Creating a common Vision is essential. Thomas Edison is quoted as saying “Vision without execution is hallucination.” My expertise in leading physician alignment and integration strategies leads me to believe: “Vision without execution is worse than having no vision at all.”
A vision of developing highly integrated, well-coordinated and person-centric care is essential to success in today’s healthcare market. Best practice in integration and alignment will begin with key stakeholder engagement in executing organizational vision. Physicians, as key stakeholders in care delivery, respond well to a establishing a common vision. Healthcare organizations that focus on a vision of “maximizing success in the ever-evolving healthcare industry through physician alignment and integration” will ultimately build capability to meet and exceed consumer expectations in navigating the path to value-based care.
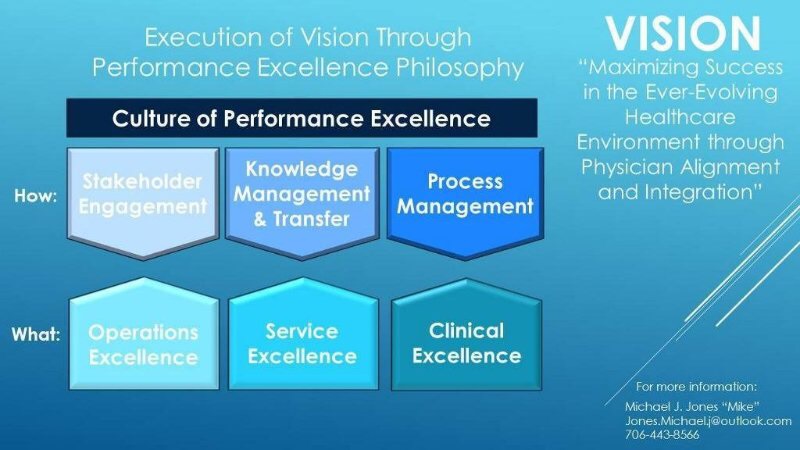
As previously highlighted in Achieve Results through Physician Alignment, Integration and Engagement: Governance and Value-based Care is Here to Stay, multiple organizational gaps may contribute to not fully realizing a vision of success in a high performing integrated delivery system. This article expands on development of a philosophy of performance excellence to achieve a vision of success. The schematic shown above provides a roadmap for navigating the performance excellence journey toward becoming a fully integrated and well-coordinated care delivery system, focused on the value-based equation of healthcare.
Vision and Execution
Today’s ever-evolving healthcare industry requires a comprehensive vision of performance excellence:
- Operating/Financial Excellence (low cost, highly efficient and cost effective service delivery),
- Service Excellence (service delivery exceeding patient and family expectations), and
- Clinical Excellence (best clinical outcomes for every patient and patient population).
More importantly execution of that vision is imperative. Most healthcare organizations have developed a vision of service delivery that meets the value-based equation of operating/financial, service and quality excellence. Direct employment of physicians and other providers is one model of integration. Other models, including developing a Clinically Integrated Network, create other opportunities for integration and alignment. Either way, it is essential to build a culture of inclusion
Execution of an organization’s vision for the future is best achieved through fostering and developing a culture of comprehensive performance excellence. Measurable results are achieved when time and energy are devoted to:
- Key Stakeholder Engagement,
- Knowledge Management/Knowledge Transfer through data analytics, and
- Formal Process Management.
Physicians, as irreplaceable key stakeholders in care delivery, should be engaged in decision making and in charting the course for success. Physicians and other key stakeholders can quickly become disenfranchised when the vision of integration is not well executed. Having physicians actively engaged at the table to participate in decision making is essential. Whether healthcare organizations are focused on growing and developing an employed physician network, or seeking to align and integrate through other means, physicians should be formally and informally engaged in:
- Governance,
- Leadership, and
- Management.
Previous articles addressed physician engagement in Governance of the Physician Enterprise Organization. This article focuses on physician engagement in Leadership and Management.
Leadership and Management:
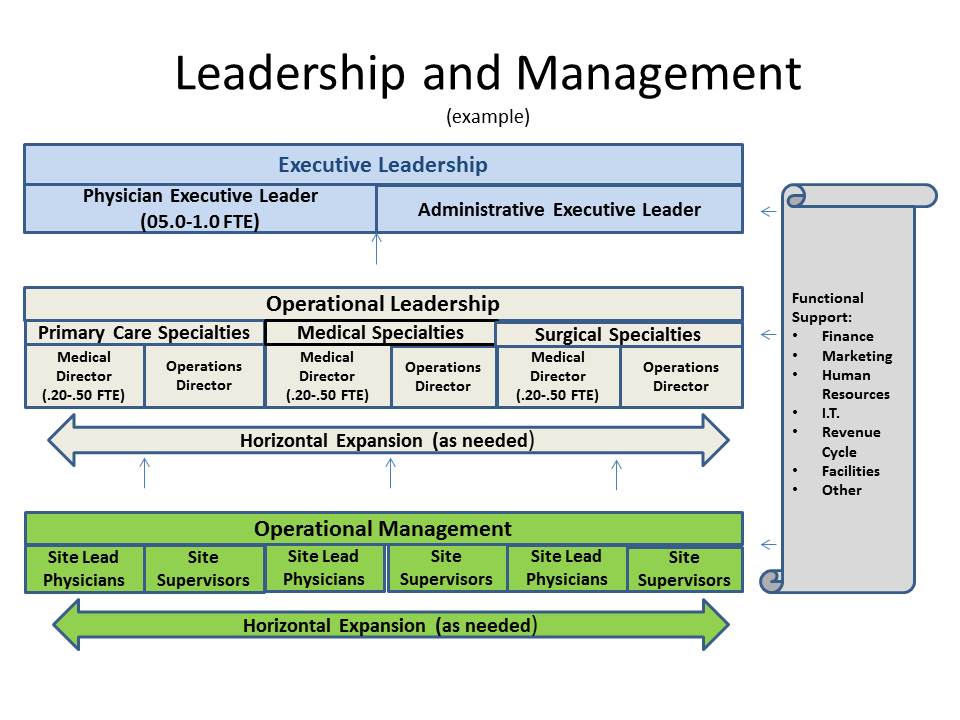
In addition to active engagement in governance, physician leadership and management is recommended. A dyad leadership model fosters a culture of engagement among physicians and support staff. The model includes physician leaders and operational leaders working in partnership at all levels:
- Executive Leadership (Physician Executive Leader and Administrative Executive Leader),
- Operational Leadership (Medical Directors and Operations Directors), and
- Operational Management (Site Lead Physicians and Operations Managers).
Physician leaders and managers in the dyad leadership model typically maintain an allocated time in clinical activities, in addition to allocated time in leadership/management activities. The prorated allocation of leadership/management time should be tailored to scope of responsibility and accountability.
An Operating Team, comprised of dyad partners at the executive and operational leadership level, should meet on a routine basis (weekly or bi-weekly) as a team to share ideas and build consistency within the physician enterprise. The Operating Team maintains accountability and responsibility for translating organization-wide goals and objectives to action. The team ensures that strategy is translated into operations. Action plans and tactics are developed to achieve strategic and operational results.
The Operating Team should meet with Site Lead Physicians and Site Supervisor/Managers on a routine basis to hard-wire operating norms. Regularly scheduled meetings of all Site Lead Physicians and Site Supervisors/Managers provide an opportunity to share best practices, build consistency and to give the practices a sense of being part of a group practice, as opposed to being isolated in individual practices.
Executive and operational leadership team members should develop a routine of rounding at all practice locations. Building relationships with practicing physicians, other providers and support staff is essential. Day to day problem solving is best achieved through active engagement of leadership, management and staff. Those who are closest to the delivery of care typically have the most innovative ideas for how best meet the needs of patients/communities services. Routine rounding also provides the opportunity for leadership to engage with patients and families to gain a better understanding of the patient experience.
An example organizational chart is provided below to give direction to leadership and management structure (see below). It should be noted that functional structure and infrastructure in the organization is most effective with limited layers of leadership and management, maintaining active relationships between leadership and staff. The organizational model is designed to expand horizontally, as opposed to vertically through creation of additional layers. Operational leadership should be tailored to the scope and diversity of specialty types within the group.
Support functions are essential to success of the physician enterprise. Finance/Accounting, Revenue Cycle, Marketing/Public Relations, Information Technology, Human Resources, Facilities/Maintenance, Purchasing and other support functions may be centralized on an enterprise-wide basis or may be structured in direct support of the physician enterprise. It should be noted that functions are highly specialized in support of a physician enterprise. Whether centralized or in direct support of the physician enterprise, it is essential for operational and executive leadership to engage directly with leadership and management of the support functions to develop a common understanding of organizational needs and performance expectations. It is recommended for support functions to be actively engaged with governance sub-committees.
Key Take Aways:
- Active engagement of key stakeholders is essential to fostering a culture of performance excellence
- Physicians can quickly become disenfranchised when not engaged in developing organizational vision
- Physician engagement and satisfaction in improved when organizational vision is well executed
- Execution is best achieved when the organization is focused on performance excellence in operations, service and clinical activities
- Developing and Fostering a culture of performance excellence requires governance, leadership and management
Next Steps:
- Knowledge management and transfer through data analytics:
- Determine the most important operational, service and clinical data analytics needed
- Process Management through formal methodologies:
- Determine the process management for the organization
- Develop leadership, management and staff to focus on processes to:
- achieve results,
- standardize operating norms,
- reduce variation, and
- hardwire best practices.
Connect with us on LinkedIn and join our Active Network Program.
