Introductory Comments:
The healthcare industry is at a crossroads. Consumerism, regulatory requirements, payer requirements, employer demands and other factors are driving forces for change in service delivery. Now is the time to get it right. We need to reduce cost, control utilization, streamline delivery of care, deliver care in a manner that exceeds patient expectations at all times, manage the health status of the communities we serve and demonstrate continuous improvement in achieving best in class clinical outcomes.
The industry, as a whole, needs to focus on the “Triple Aim” (low cost, service oriented and high quality). In doing so, we cannot neglect that we can only navigate the course to achieving value based results with a high performing team of leadership representatives, management representatives, physicians, other clinical providers and staff, thus achieving the “Quadruple Aim.”
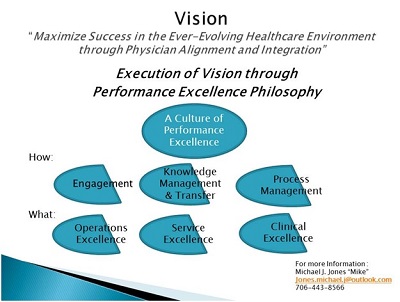
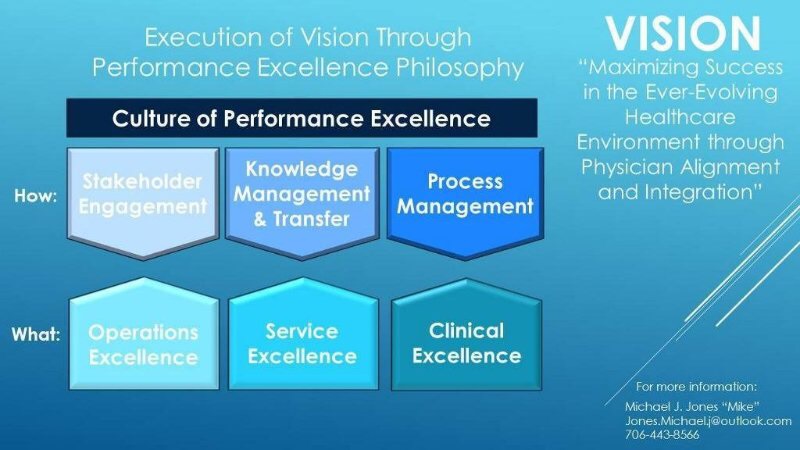
We must engage and empower our clinical and non-clinical workforce to maintain professional satisfaction and reduce the risk of burn-out from expecting more without addressing resource requirements. It is not easy, but it can be framed in a simplified philosophy of Performance Excellence. Performance Excellence (Operations, Service and Clinical) is the gold standard by which healthcare teams will be measured.
Is your physician enterprise designed to allow every member of your organization to autograph their work with excellence?
Workforce (physicians, advanced practice providers, clinical and non-clinical staff) engagement at all levels of your organization is essential to move forward in today’s ever-evolving healthcare market. A Performance Excellence Philosophy provides the systematic methodology to engage your workforce in achieving results.
The Baldrige Excellence Framework (Healthcare): As Systems Approach to Improving Your Organization’s Performance empowers your organization to reach its goals, improve results, and become more competitive. The framework consists of the criteria, the core values and concepts, and scoring guidelines to use as reference, to self-assess, or as a basis for external assessment. Whether or not your organization is “award and recognition oriented,” today’s ever-evolving healthcare environment creates to perfect opportunity to take a step back and assess your ability to achieve value based results.
Through active inquiry regarding your organization’s culture, you learn and develop your ability to accomplish what is important to your organization. A community/customer/patient centered philosophy, along with the critical aspects of: Leadership/Governance; Vision/Strategy; Measurement, Analysis, and Knowledge Management (through data analytics); and Operational Work Processes and Process Management, allows you to evaluate how prepared you are to achieve VALUE BASED RESULTS.
Through internal ASSESSMENT you may find that your organization needs external resources to develop the necessary structure and infrastructure to achieve your VISION. Experienced leadership with a demonstrated track record of achieving results within physician enterprise organizations may be difficult to find. You may need Interim Leadership and Management Advisory Services with the Resilience to do the “initial heavy lifting” of positioning your enterprise for high performance.
Today we explore ways to assess your systematic approach for delivering value in your communities.
Assess Your Physician Enterprise through a Systematic Approach
Vision:You need a systematic approach to assessing your physician enterprise ability to achieve results. You need a framework to deliver value. The challenge is to critically assess to learn how you are accomplishing your vision and strategic priorities. Today we pose several key questions to begin to assess your organization’s readiness to achieve value based results.
Has your organization set a strategic priority for achieving value based results in your physician enterprise?
How has your organization set a strategic priority for achieving value based results? “Value Based Care is Here to Stay”:
Vision and Strategy-Questions to consider:
Is it important to your organization?
Have you established a shared Vision of physician integration to achieve value based results?
Is your organization prepared to create greater value in the communities you serve?
Does your organization have the leadership with the demonstrated competency of RESLIENCE to navigate the path to value?
Do you need Interim Leadership or experienced external advisors to assess and develop your physician enterprise ability to deliver value based results
Please see Assessing Your Vision and Strategies, to begin your assessment: You may also request a copy from: This email address is being protected from spambots. You need JavaScript enabled to view it.
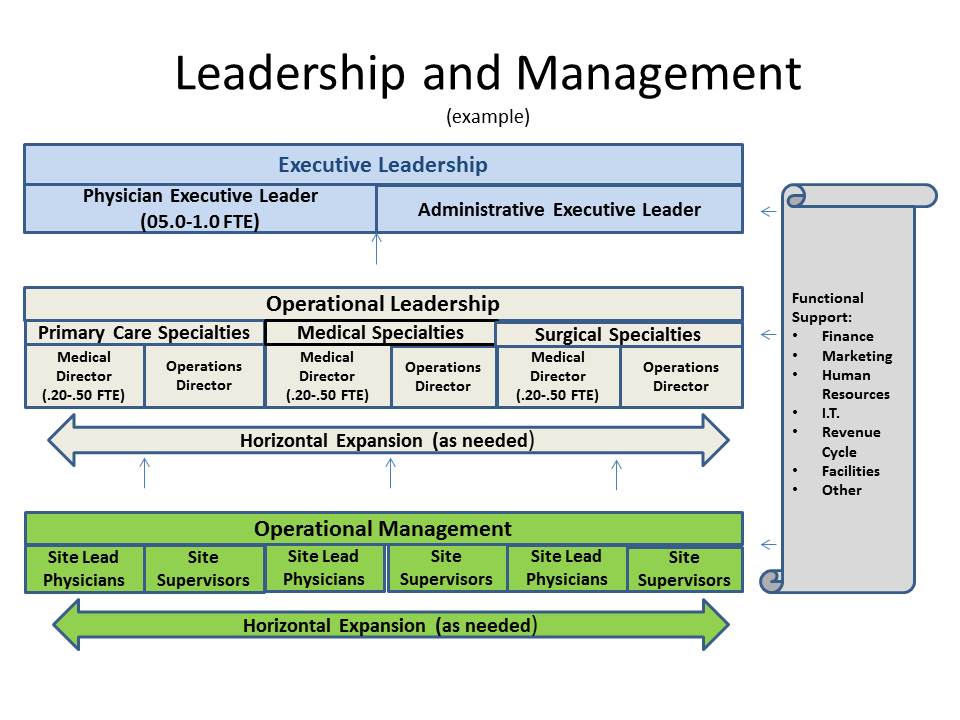
It all begins with LEADERSHIP:
Leadership must promote a systems perspective. A systems perspective means managing all the components of your organization as a whole to achieve ongoing success. A healthcare system has many inter-related, but not always highly integrated, components. Each component must be led and managed to function as a high performing organization within the context of the entire system. Most importantly, your physician enterprise (whether an employed network or Clinically Integrated Network) must demonstrate a successful track record of achieving results.
Assess your leadership and management structure to achieve results:
“Achieve Results-Leadership and Management”
Question to Consider-Leadership:
Do senior leaders lead the organization, consistent with your systematic approach?
Please see Assessing Your Leadership/Management, to begin your assessment: You may also request a copy from: This email address is being protected from spambots. You need JavaScript enabled to view it.
Governance:
How does your governance structure oversee your physician enterprise and address your organizational ability to achieve value based results?
Assess your governance structure to achieve results: "Governance”
Governance - Questions to Consider:
How does your organization ensure responsible governance of the physician enterprise?
How does your governing achieve accountability for:
- senior leaders’ actions
- strategic plans
- fiscal accountability
- transparency in operations
- selection of governance board members and disclosure policies for them, as appropriate
- independence and effectiveness of internal and external audits
- protection of stakeholder and stockholder interests, as appropriate
- succession planning for organizational leadership
Please see Assessing Your Governance, to begin your assessment: You may also request a copy from: This email address is being protected from spambots. You need JavaScript enabled to view it.
Knowledge Management/Transfer through Data Analytics:
How do you measure, analyze, and then improve organizational performance?
Assess your Performance Measures to achieve results: "Knowledge Management/Transfer through Data Analytics”
Questions to Consider - Performance Measures:
How do you track data and information on daily operations and overall organizational performance?
How do you select, collect, align, and integrate data and information to use in tracking daily operations and overall organizational performance; and track progress on achieving strategic objectives and action plans?
Please see Assessing Your Knowledge Management/Transfer through Data Analytics, to begin your assessment: You may also request a copy from: This email address is being protected from spambots. You need JavaScript enabled to view it.
Operations Management/Process Management:
How do you design, manage and improve your key health care services and work processes?
Assess your Work Processes/Process Management Methodology to achieve results: “Process Management-Achieve Value Based Results”
Questions to Consider-Work Processes/Process Management:
How do you design, manage, and improve your key health care services and work processes?
How do you determine key health care service and work process requirements?
Please see Operations Management/Process Management, to begin your assessment: You may also request a copy from: This email address is being protected from spambots. You need JavaScript enabled to view it.
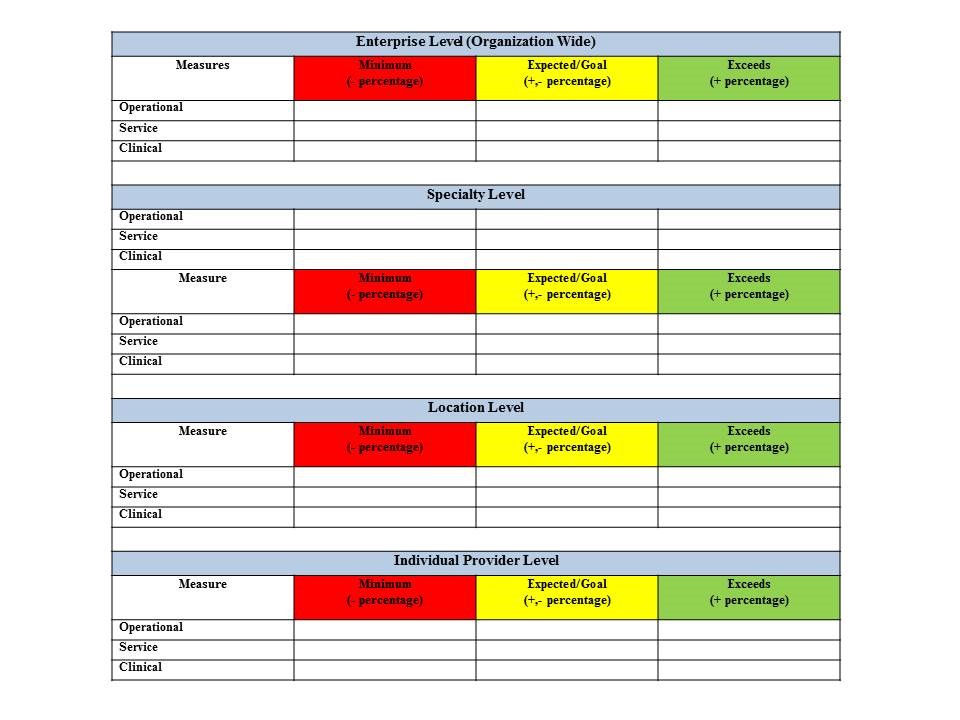
Results:
A Performance Excellence Philosophy provides the systematic methodology to achieve results. Your organization will achieve value based results with unrelenting commitment from key stakeholders at every level.
You need a simplified approach to creating a culture of Performance Excellence to achieve results:
Question to Consider-Results
What are your health care and process effectiveness results?
What are your health care results and your results for your patient and other customer service processes?
Is your entire workforce engaged in achieving value based results?
Please see Assessing Your Results, to begin your assessment:
Key Take Aways and Next Steps:
- Assess and adopt a Vision of Value Based Care in your Physician Enterprise
- Implement a Culture of Performance Excellence
- Assess your Leadership/Management
- Assess your Governance
- Assess your Knowledge Management/Transfer (Data Analytics)
- Assess your Operations/Process Management
- Assess your Results
- You may need external resources to assist in assessment and development




 Hardwire/Standardize best practice, process design to ACHIEVE
Hardwire/Standardize best practice, process design to ACHIEVE 

 Click
Click