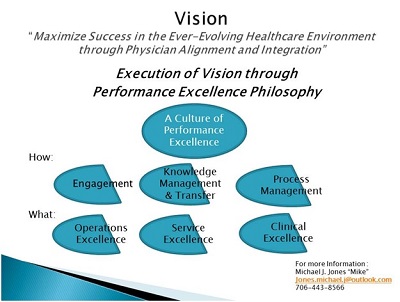
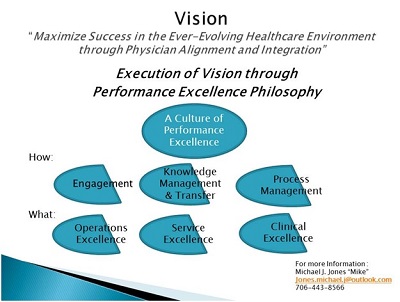
Culture of Performance Excellence: A simplified Approach
Physician alignment, integration and engagement in integrated delivery systems are essential elements in navigating the complexity of healthcare service delivery. Healthcare organizations need a simplified approach to realize organizational vision of comprehensive and successful alignment and integration strategies. Creating a common Vision is essential. Thomas Edison is quoted as saying “Vision without execution is hallucination.” My expertise in leading physician alignment and integration strategies leads me to believe: “Vision without execution is worse than having no vision at all.”
A vision of developing highly integrated, well-coordinated and person-centric care is essential to success in today’s healthcare market. Best practice in integration and alignment will begin with key stakeholder engagement in executing organizational vision. Physicians, as key stakeholders in care delivery, respond well to a establishing a common vision. Healthcare organizations that focus on a vision of “maximizing success in the ever-evolving healthcare industry through physician alignment and integration” will ultimately build capability to meet and exceed consumer expectations in navigating the path to value-based care.
As previously highlighted, multiple organizational gaps may contribute to not fully realizing a vision of success in a high performing integrated delivery system. This article expands on development of a philosophy of performance excellence to achieve a vision of success. The schematic shown above provides a roadmap for navigating the performance excellence journey toward becoming a fully integrated and well-coordinated care delivery system, focused on the value-based equation of healthcare.
Vision and Execution
Today’s ever-evolving healthcare industry requires a comprehensive vision of performance excellence:
- Operating/Financial Excellence (low cost, highly efficient and cost effective service delivery),
- Service Excellence (service delivery exceeding patient and family expectations), and
- Clinical Excellence (best clinical outcomes for every patient and patient population).
More importantly execution of that vision is imperative. Most healthcare organizations have developed a vision of service delivery that meets the value-based equation of operating/financial, service and quality excellence. Direct employment of physicians and other providers is one model of integration. Other models, including developing a Clinically Integrated Network, create other opportunities for integration and alignment. Either way, it is essential to build a culture of inclusion.
Execution of an organization’s vision for the future is best achieved through fostering and developing a culture of comprehensive performance excellence. Measurable results are achieved when time and energy are devoted to:
- Key Stakeholder Engagement,
- Knowledge Management/Knowledge Transfer through data analytics, and
- Formal Process Management.
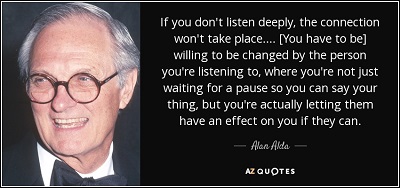
Physicians, as irreplaceable key stakeholders in care delivery, should be engaged in decision making and in charting the course for success. Physicians and other key stakeholders can quickly become disenfranchised when the vision of integration is not well executed. Having physicians actively engaged at the table to participate in decision making is essential. Whether healthcare organizations are focused on growing and developing an employed physician network, or seeking to align and integrate through other means, physicians should be formally and informally engaged in:
- Governance,
- Leadership, and
- Management
This article focused on physician engagement in Governance of a Physician Enterprise Organization. The article in this series will focus on establishing Leadership and Management Structure to execute the organizational vision.
Governance:
Hospital organizations have been inviting physicians to be members of governance structures for many years. In addition to representing medical staff activities, physicians can help foster a physician friendly culture at the board level. Gaining the physician perspective of hospital operations and embracing input will contribute to an environment of high performance. Physicians are typically viewed as customers of hospital based services.
Governance within a physician enterprise organization (employed model or clinically integrated network) requires a very high level of engagement among physicians. Physician enterprise organizations have a profound impact on a physician’s practice and physician’s entire livelihood. A high level of governance to oversee and provide direction is needed. A physician led governing board is recommended. Physicians should be viewed as key stakeholders and leaders in care delivery.
While physician governance is recommended, organizations may adopt a formal governing body with corporate bylaws which define scope of responsibility and accountability, or less formal governance oversight in an advisory capacity. Scope of responsibility and accountability of the physician led governance and reserved powers of higher governing authority at a system-wide level must be clearly defined. The majority of governing body membership should be comprised of physician members with predetermined representation from medical and surgical specialties from within the group. Administrative leadership is tasked with facilitating and directing physician governance through a high level of trust and credibility.
The Governing Body of a physician enterprise organization may be structured to include the physician led board, as well as several sub-committees with defined functional oversight as defined by committee charters:
- Policy and Procedure
- Regulatory Compliance
- Physician/Provider expectations:
- Productivity
- Access
- Guiding principles related to citizenship and behavioural standards
- Quality performance
- Service performance
- Operational/Financial performance.
Sub-committees of the governing board are recommended to foster a broader level of engagement and participation among physician members of the group. The board may consider delegation of oversight to subcommittees to create focus and subject matter expertise through measuring, monitoring, reporting and improving performance. Sub-committees to consider include:
- Finance Committee
- Oversight of provider productivity
- Oversight of financial measures
- Capital allocation and approval
- Oversight of Revenue Cycle
- Clinical Quality Committee:
- Regulatory required quality reporting
- Non-regulatory quality improvement activities
- Growth Committee:
- Growth Committee
- Provider manpower planning
- Provider recruitment and selection
- Provider retention
- Provider engagement and satisfaction
- New service development
- Service Excellence/Patient Experience Committee:
- Patient experience survey process
- Patient experience expectations
- Patient experience improvement initiatives
- Informatics and Automation Committee:
- System selection
- System implementation
- System performance and optimization
- Physician Compensation Committee
- Create a common understanding of fair market value for physician compensation models
- Create incentive based compensation and align with value
- Communicate broadly among all physician members of the group
- Payer Relations and Contracting Committee:
- Contract negotiation
- Engagement in value-based initiatives
Key Take-Aways:
- Active engagement of key stakeholders is essential to fostering a culture of performance excellence
- Physicians can quickly become disenfranchised when not engaged in developing organizational vision
- Physician engagement and satisfaction in improved when organizational vision is well executed
-
Execution is best achieved when the organization is focused on performance excellence in operations, service and clinical activities
- Developing and fostering a culture of performance excellence requires physician engagement Governance of the Physician Enterprise
Next Steps:
- Assess and design the Leadership and Management structure of the physician enterprise to enhance the performance excellence culture
-
Knowledge management and transfer through data analytics:
- Determine the most important operational, service and clinical data analytics needed
-
Process Management through formal methodologies:
- Determine the process management for the organization
- Develop leadership, management and staff to focus on processes to:
- achieve results,
- standardize operating norms,
- reduce variation, and
- hardwire best practices.
Connect with Mike on LinkedIn.
Connect with us on LinkedIn and join our Active Network Program.