“If you can’t describe what you are doing as a process, you don’t know what you are doing.” Such a profound quote by W. Edwards Deming, largely recognized as the Father of the Quality Movement. Dr. Deming's famous 14 Points, originally presented in Out of the Crisis, serve as management guidelines. The points cultivate a fertile soil in which a more efficient workplace, higher profits, and increased productivity may grow. These management principles have a direct correlation to navigating the path to achieving results in the uncertain healthcare industry of today.
Deming’s 14 Points for Leadership/Management
While traditionally applied to product manufacturing, Deming theory has direct application across multiple industries, especially when rising consumer and regulatory requirements demand greater value. View healthcare service delivery as a product in high demand from consumers (patients, families and others). Expectations of lower cost and superb quality, delivered in a highly patient-centric and service-oriented environment, create an imperative healthcare systems must meet to remain relevant.
Healthcare leaders are served well when focusing on Deming’s 14 Points:
- Create constancy of purpose toward improvement of product and service, with the aim to become competitive, to stay in business and to provide jobs.
- Adopt the new philosophy. We are in a new economic age. Western management must awaken to the challenge, must learn their responsibilities, and take on leadership for change.
- Cease dependence on inspection to achieve quality. Eliminate the need for massive inspection by building quality into the product in the first place.
- End the practice of awarding business on the basis of a price tag. Instead, minimize total cost. Move towards a single supplier for any one item, on a long-term relationship of loyalty and trust.
- Improve constantly and forever the system of production and service, to improve quality and productivity, and thus constantly decrease costs.
- Institute training on the job.
- Institute leadership (see Point 12 and Ch. 8 of Out of the Crisis). The aim of supervision should be to help people and machines and gadgets do a better job. Supervision of management is in need of overhaul, as well as supervision of production workers
- Drive out fear, so that everyone may work effectively for the company. (See Ch. 3 of Out of the Crisis).
- Break down barriers between departments. People in research, design, sales, and production must work as a team in order to foresee problems of production and usage that may be encountered with the product or service.
- Eliminate slogans, exhortations, and targets for the work force asking for zero defects and new levels of productivity. Such exhortations only create adversarial relationships, as the bulk of the causes of low quality and low productivity belong to the system and thus lie beyond the power of the work force.
- Eliminate work standards (quotas) on the factory floor. Substitute with leadership.
- Eliminate management by objective. Eliminate management by numbers and numerical goals. Instead substitute with leadership.
- Remove barriers that rob the hourly worker of his right to pride of workmanship. The responsibility of supervisors must be changed from sheer numbers to quality.
- Remove barriers that rob people in management and in engineering of their right to pride of workmanship. This means, inter alia, abolishment of the annual or merit rating and of management by objectives (See Ch. 3 of Out of the Crisis).
- Institute a vigorous program of education and self-improvement.
- Put everybody in the company to work to accomplish the transformation. The transformation is everybody's job.
The focus of this article is to bring home the reality that EVERYTHING IS A PROCESS. “If you cannot describe what you are doing as process, you do not know what you are doing.”
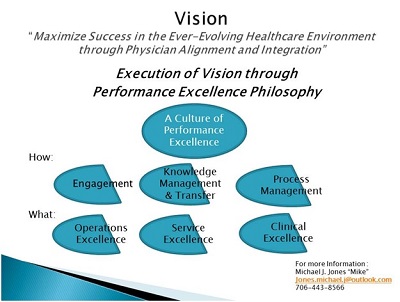
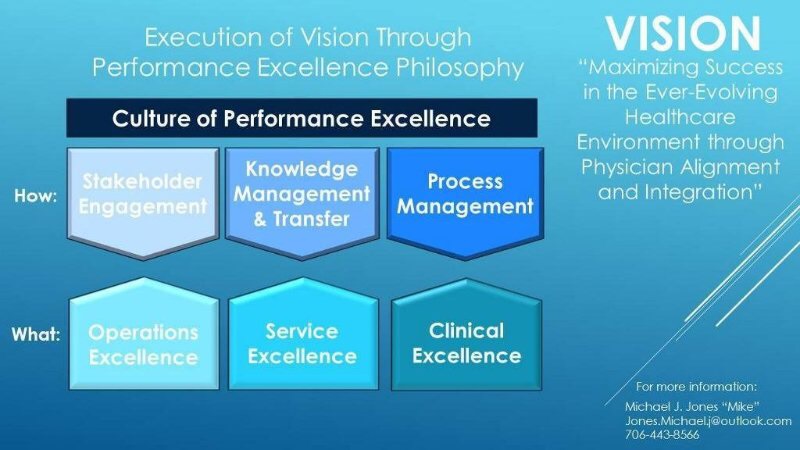
Physician alignment, integration and engagement in integrated delivery systems are essential elements in navigating the complexity of healthcare service delivery. Healthcare organizations need a simplified approach to realize organizational vision of comprehensive and successful alignment and integration strategies. Creating a common Vision is essential. Healthcare organizations that focus on a vision of “maximizing success in the ever-evolving healthcare industry through physician alignment and integration” will ultimately build capability to meet and exceed consumer expectations in navigating the path to value-based care. Today’s ever-evolving healthcare industry requires a comprehensive Vision of Integration. Execution of the Vision is best achieved through a Leadership Philosophy of Performance Excellence.
The first key element in fostering a culture of performance excellence is to define the “WHAT” that constitutes excellence, frequently referred to as “the Triple Aim” of healthcare:
- Operating/Financial Excellence (low cost, highly efficient and cost effective service delivery),
- Service Excellence (service delivery exceeding patient and family expectations), and
- Clinical Excellence (best clinical outcomes for every patient and patient population).
The next essential element of a performance excellence culture is to define the “HOW” the organization will be led through:
- Stakeholder Engagement
- Knowledge Management/Knowledge Transfer
- Process Management
Organizations will not only achieve the “triple aim”, but will enhance performance through achieving the “quadruple aim” of healthcare. In addition to achieving traditional value-based results, a culture of performance excellence will yield higher levels of provider satisfaction and engagement while redefining service delivery. As highlighted in previous articles:
-
Value Based Care is here to stay and healthcare organizations must overcome multiple organizational gaps that may contribute to not fully realizing a vision of success in a high performing integrated delivery system. Here
-
Key Stakeholder Engagement is essential to execution of a common Vision:
-
Physician Stakeholders (as well as others) should be engaged in organizational Governance, especially among healthcare providers, is essential to success in a value based environment. Here.
-
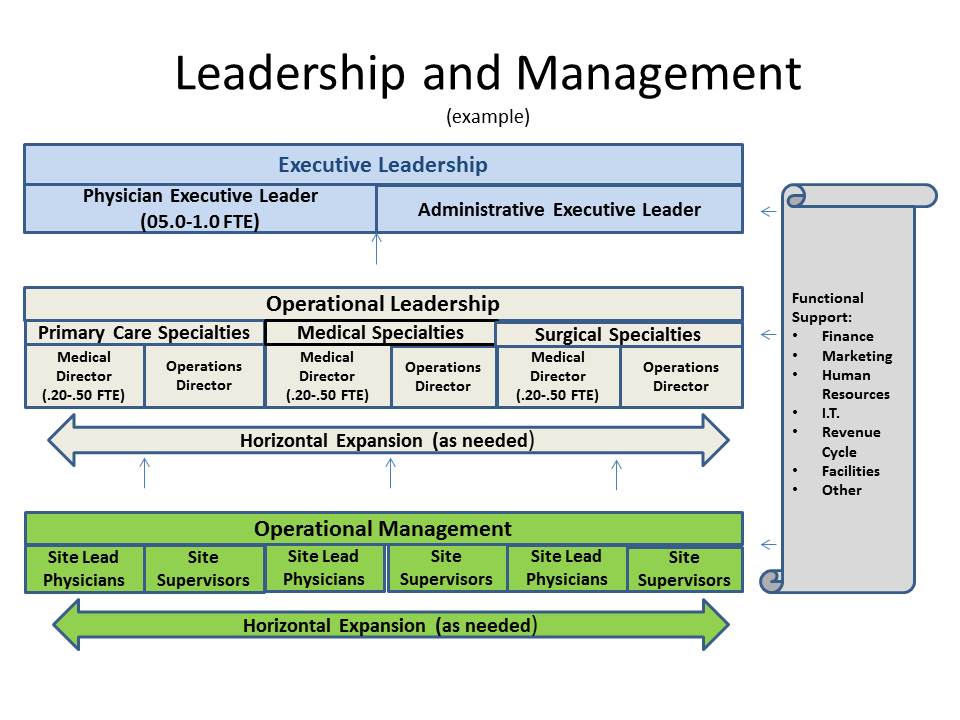
Physician Stakeholders should also be engaged in Leadership and Management to achieve sustainable results. Here.
- Knowledge Management/Knowledge Transfer
-
A common understanding of performance is best achieved through measuring, monitoring, reporting and analysis of key outcomes: Operational, Service and Clinical Metrics (Data Analytics) Here.
- Opportunities for performance improvement are quickly identifiable when using data analytics in evaluating current outcomes.Here.
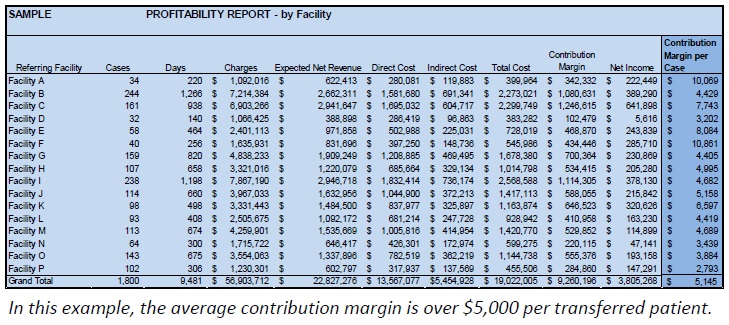
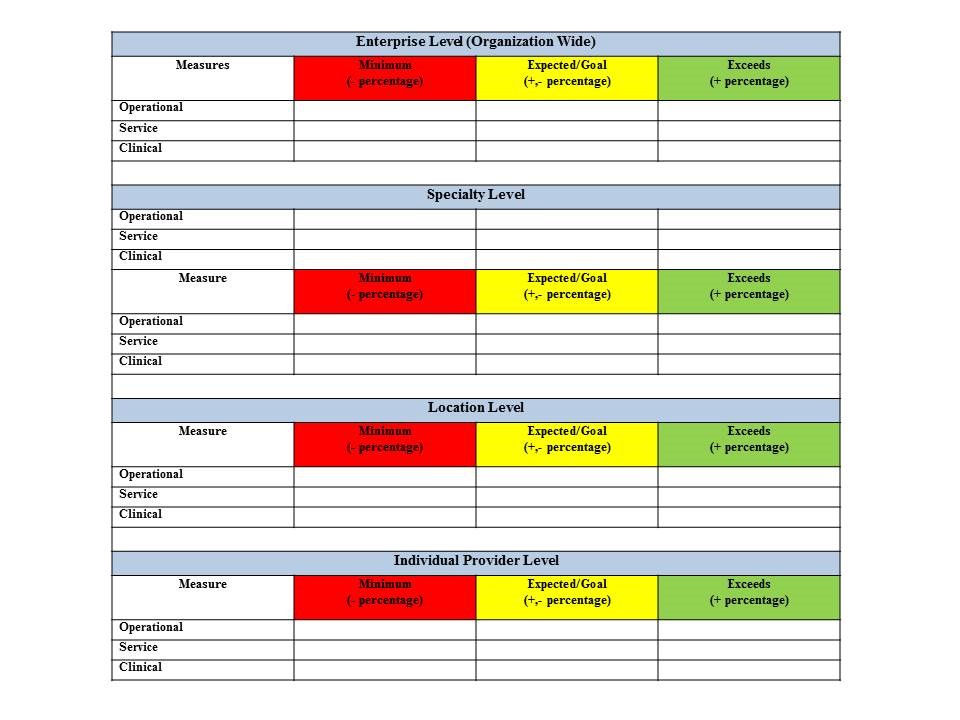
This article expands on development of a Philosophy of Performance Excellence to achieve a vision of success through Performance Management. Measuring, monitoring, reporting, analyzing and improving performance begins with defining key metrics to create a common understanding. Internal and external benchmark measures are available through a variety of sources to build an improved understanding of: Operational/Financial, Service, and Clinical Performance. Now you need a methodology to achieve your desired outcomes.
Physicians and other care providers work within a defined process everyday of their lives when addressing and resolving patient needs for care. What is done when presented with multiple patients with complex healthcare needs? SOAP is a traditional approach to addressing patient needs:
The SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by health care providers to write out notes in a patient's chart, along with other common formats, such as the admission note. Documenting patient encounters in the medical record is an integral part of practice workflow starting with patient appointment scheduling, to writing out notes, to medical billing. The SOAP note originated from the Problem Oriented Medical Record (POMR), developed by Lawrence Weed, MD.[1] It was initially developed for physicians, who at the time, were the only health care providers allowed to write in a medical record. Today, it is widely adopted as a communication tool between inter-disciplinary healthcare providers as a way to document a patient’s progress. SOAP notes are now commonly found in electronic medical records (EMR) and are used by providers of various backgrounds. Prehospital care providers such as EMTs may use the same format to communicate patient information to emergency department clinicians. Physicians, physician assistants, nurse practitioners, pharmacists, podiatrists, chiropractors, acupuncturists, occupational therapists, physical therapists, school psychologists, speech-language pathologists, certified athletic trainers (ATC), sports therapists, occupational therapists, among other providers use this format for the patient's initial visit and to monitor progress during follow-up care.
It is a well-defined thought process. Complete a SUBJECTIVE EVALUATION, an OBJECTIVE EVALUATION, an ASSESSMENT and a PLAN. Engage patients and family members when seeking to understand what is happening with a patient (Subjective). Gather facts/data regarding what is happening with a patient through diagnostic procedures (Objective). Review the information gathered and knowledge gained from the evaluations (Assessment) and take action to address what has been presented (Plan). Why not apply a similar process that is highly effective to leadership and management. That is a process management/performance management approach.
Performance Management
The days of simply making claims of high-quality, service-oriented and low cost care delivery are gone. Patients, families, communities, payers, regulatory agencies and other key stakeholders demand proof of performance. Measures of performance should focus on Operations/Financial, Service and Clinical Excellence. Internal and external benchmarking of performance is imperative. Once you understand current performance through data analytics, you need tools to achieve continuous improvement.
There are many theories of performance/process management. Theories and practices have evolved over time. Many are inter-related and draw on common practices. Process Management philosophies include, but are not limited to:
- Total Quality Management (TQM):
- Focus on the Consumer
- Continuous Improvement
- Quality Improvement
- Accurate Evaluation
- Continuous Quality Improvement (CQI):
-
Plan Do Study Act (PDSA): Model for Improvement: What are we trying to accomplish? How will we know that a change in an improvement? What change can we make that will result in improvement?
- Plan: Objective, Questions and Predictions, Plan to carry out the cycle (who, what, where, when)
- Do: Carry out the plan. Document problems and unexpected observations. Begin data analysis.
- Study: Complete the data analytics. Compare data to predictions. Summarize what you have learned.
- Act: What changes are to be made? Begin the next cycle.
- Lean Management:
- Leadership Commitment to Project (s)
- Project Charter (Standardized for ease of understanding).
- Project Tracking (verify milestones)
- Assign Project Manager
- Engage Key Stakeholders
- Communicate Frequently
- Achieve Results
- Lean:
- Waste Reduction
- Continuous Improvement
- Respect for People
- Six Sigma-DMAIC:
-
Define: Define project purpose and scope. Identify high level processes for improvement. Determine customer needs and benefits.
-
Measure: Baseline data on current processes. Pinpoint problem locations and occurrences. Identify potential areas for improvement.
-
Analyse: Identify root causes and validate root causes against captured data. Determine improvements that need to be made.
-
Improve: Implement the improvements that have been determined to address the root causes.
-
Control: Perform before and after analysis. Monitor processes/systems. Document results. Determine next steps/recommendations.
- Lean/Six Sigma:
-
Lean: focuses on waste reduction by streamlining process
-
Six Sigma: focuses on preventing defects through problem solving
-
Lean/Six Sigma: Lean strengthens Six Sigma-Problem solving plus improving process delivers greater value-based results
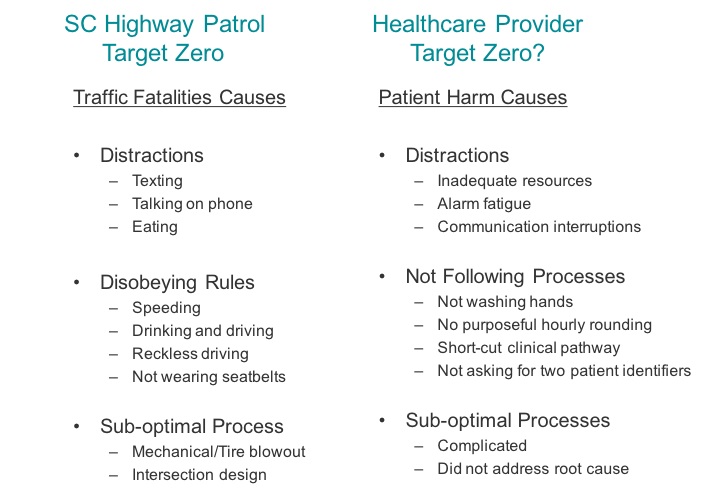
The common thread in all methodologies is an unrelenting focus on seeking improved outcomes in everything we do:
- Cycles of improvement
- Engaging in a customer focus
- Understanding key stakeholder perspective
- Measuring current performance through data analytics
- Engaging those closest to the work:
- to define current processes (value stream mapping, flowcharting)
- to define desired outcomes of current processes
- to define undesirable outcomes (failures) of current process
- identify and define best practices
- identify and define outcomes
- identify and define preferred processes to achieve best practice performance and outcomes
- transfer best practices, best practice outcomes and preferred processes to:
- gain consistency across all players
- reduce variation in outcomes and results across all players
- meet and exceed customer expectations at all times
- reduce cost of service delivery
- increase throughput in service delivery
- provide consistent, high-quality outcomes
Performance Management Simplified
High performing leaders in healthcare organizations of today are challenged with the uncertainty of healthcare delivery in the future. Creating a performance excellence environment is the best to navigate the ever-evolving imperatives of service delivery. Value based results will be achieved through a leadership philosophy of performance excellence:

Engage your People

Evaluate your data; identify best practice

Know your process and design your process
 Hardwire/Standardize best practice, process design to ACHIEVE
Hardwire/Standardize best practice, process design to ACHIEVE 
Key Take Aways:
- You have highly engaged employees, physicians, patients, family members, community representatives and payers.
- You have defined a common and shared vision for your organization through gaining knowledge of your key stakeholders’ perspectives
- You have defined what outcomes you and your organization are trying to achieve in terms of Operations, Finance, Service and Clinical indicators
- You have measured your current performance
- Now you want to improve performance:
- Everything is a process
- Gain an understanding of your current processes
- Identify your best practices
- Design process to achieve best practice performance
- Re-evaluate your performance to see if you are consistently achieving improved performance
- Modify your processes when necessary to consistently achieve higher levels of performance
- Hard-wire your processes to ALWAYS achieve best practice performance
- Never stop monitoring to verify your preferred state performance/outcomes.
- Pick a methodology for process management (they all work)
- Train for it
- Build consistency of approach
Next Steps:
- Define your performance excellence culture
- Relentless leadership focus on performance excellence
- Adopt your preferred methodology
- Formalize and standardize your methodology
- Listen to your key stakeholders
- Engage all parties in understanding improvement initiatives
- Gain understanding of performance through data analytics
- Design processes to achieve desired results
- Achieve success in all you do
- Demonstrate that you are creating value based outcomes



 Hardwire/Standardize best practice, process design to ACHIEVE
Hardwire/Standardize best practice, process design to ACHIEVE 










 Click
Click